Interventional Radiology
Interventional Radiology (abbreviated IR or sometimes VIR for vascular and interventional radiology) http://en.wikipedia.org/wiki/Interventional_radiology
Interventional Radiologists are a sub-specialized core of Radiologists who use state of the art imaging equipment (X-ray, CT, MRI, or Ultrasound) to perform a vast array of advanced diagnostic and therapeutic procedures. TRA Interventional Radiologists work closely with referring physicians to provide minimally invasive, targeted treatments, often times reducing the need for surgery. These procedures are often performed in an outpatient setting, resulting in lower cost, lower risk, less pain, and a shortened recovery time. TRA Interventional Radiologists are experts in Angiography (catheterizing and treating blocked arteries and veins), image guided biopsy of deep and hidden masses in the body, ablation and chemo-embolization of tumors in the liver, kidneys, lungs, etc. Our Intereventionalists have trained and held faculty positions at some of the most respected/premier programs in the country, including University of Michigan, Massachusetts General Hospital and Cleveland Clinic. TRA Intereventionalists have introduced several new procedures to the Northwest Ohio and Southeastern Michigan area including Vertebroplasty, Kyphoplasty, Uterine Fibroid Embolization, TIPS (Transjugular Intrahepatic Portosystemic Shunts), Tumor ablation, and Tumor embolization. TRA Interventional Radiologists in association with the Jobst Vascular Center worked to develop a world renowned Endograft program to treat abdominal aortic aneurysm. The TRA Interventional Radiology service in association with the Jobst Vascular Center offers unparalleled experience in the treatment of patients with deep venous thrombosis (blood clots in leg, arm and chest veins). We offer state-of-the-art treatment with an array of techniques to restore flow to occluded veins. We are actively involved in national multicenter clinical trials investigating these techniques, allowing patients, should they choose, access to techniques at the forefront of treatment of this disease. (eg., “STRIDE; “Acute Venous: Thrombus Removal With Adjunctive Catheter-Directed Thrombolysis–The ATTRACT Trial”).www.sirweb.org/clinical/cpg/617.pdf
Please browse the following descriptions to learn more about the many services we provide:
Vertebroplasty and Kyphoplasty
Uterine Fibroid Embolization (UFE)
Transjugular Intrahepatic Portosystemic Shunts(TIPS)
Vertebroplasty and Kyphoplasty:
Patients with osteoporotic spine fractures can suffer from severe, often life-limiting, back pain, kyphosis (spine curvature), and limited mobility. Vertebroplasty is a percutaneous X-ray guided technique to stabilize the fracture, and alleviate the pain; it was introduced in Europe a decade ago, and is now widely available in the US to treat painful compression spine fractures. Kyphoplasty, is a slightly modified technique that involves placing a balloon in the fractured vertebral body to restore its height, then filling the vacuum created with bone cement. Based on our experience, both procedures are very effective in alleviating pain originating from spine compression fractures. TRA Intereventionalists were among the first to bring this new treatment to Northwest Ohio, and are actively involved in national multicenter research trials to prospectively study the advantages, and differences of both techniques.
Please see link to KAVIAR trial:
- http://trialx.com/clinicaltrial/71247/spinal-fractures-kaviar-study–kyphoplasty/
- http://www.sirweb.org/medical-professionals/PIB_PDFs/Vertebroplasty.pdf

Uterine Fibroid Embolization (UFE):
Approximately 40% of women over 35 will experience some symptoms related to uterine fibroids (benign tumors of the uterus). Symptoms may include heavy menstrual bleeding, pelvic pain, anemia, frequent urination and difficulty getting pregnant. UFE is a relatively new technique which is highly effective in treating medical symptomatic fibroids without invasive surgery. Read more about UFE and fibroid treatment options at these websites:
- Fibroid Treatment Collective (www.fibroids.com)
- Society of Interventional Radiology (www.sirweb.org) (see: Fibroid Symptoms & Diagnosis)

back to page menu
Tumor Ablation:
Our Interventional Radiologists offer multiple types of tumor ablation therapy: tumors can be eradicated by radiofrequency (by heat), (Chemo ablation) (Freezing ablation) (Cryoablation)
- Chemoembolization: Using a catheter guided through a patient’s blood vessels infusing a highly concentrated chemo thru its feeding vessel.www.sirweb.org/news/newsPDF/Cancer_TACE_release.pdf
- Radiofrequency Ablation: Ablating the tumor by using a probe to deliver radiofrequency waves. www.sirweb.org/patients/lung-cancer
- Cryoablation: a process that uses extreme cold (cryo) to remove tissue (ablation). www.sirweb.org/news/newsPDF/2008am/Mon/Renal_cryoFinal.pdf
back to page menu
Venous and GI Access:
When venous access is required for such procedures dialysis, long-term chemotherapy or antibiotic therapy, various types of central lines can be placed by your Interventional Radiologist. Similarly, when GI access is required as in patients with certain types of esophageal or gastric cancer, feeding tubes may be placed. www.sirweb.org/patients/gastrostomy/
back to page menu
Vascular Stenting:
Interventional radiologists may detect a narrowing or blockage in blood vessels going to the kidneys, abdomen or extremities using a procedure called angiography. When such a narrowing is found, balloons and metallic stents may be inserted to help keep the vessel open. www.sirweb.org/patients/angioplasty-stent/
back to page menu
Image Guided Biopsy:
Some tumors or masses that cannot be felt on the skin surface require image guided biopsy to determine whether they represent cancer or a benign process. www.sirweb.org/patients/needle-biopsy/
back to page menu
Transjugular Intrahepatic Portosystemic Shunts(TIPS):
TIPS is a procedure performed by Interventional radiologist (vascular radiologists) at many major medical centers throughout the country for patients with various complications from their advanced liver disease. Initial work with the placement of TIPS devices in humans was first reported in 1982 by Colapinto but the more modern use of expandable metal mesh stents with significantly improved results was not reported till 1990 by Richter. Since 1990 refinements in technique and a growing experience with the method have made TIPS widely available in many major medical centers, particularly in liver transplant centers. This technique has offered an outstanding treatment alternative to earlier complex operations required to treat these life-threatening complications of cirrhosis.
Patients with cirrhosis develop high pressures in the main blood vessel that supplies the liver called the portal vein due to the increase resistance to blood flow in the diseased and scarred liver. A TIPS involves the creation of a tissue tract from the low pressure venous system that drains the liver to the high pressure venous system that feeds the liver in cirrhosis. The tract is made by inserting a catheter through a large blood vessel in the neck which communicates with the blood vessels draining the liver. Under X-RAY guidance, doctors are then able to establish within the substance of the liver an artificial tract or shunt to directly drain the portal vein into the general circulation. This is done via the use of several inflatable balloons followed by the careful insertion of an expandable, wire mesh stent. Doctors insert TIPS devices in patients with liver disease who have serious and life threatening complications such as the prescence of hemmorhage from the stomach or esophagus, problematic fluid accumulation in the abdomen, and also for a form of kidney failure that arises in some patients with advanced liver failure. In addition to sucessfully decompressing the portal venous system in over 95% of cases, blood flow to the kidneys frequently improves. The increased blood flow to the kidneys will not injure them and in fact can lead to an overall improvement in kidney function in some patients with cirrhosis. http://www.radiologyinfo.org/en/info.cfm?pg=tips
back to page menu
Intra-arterial Y-90 Radioembolization:
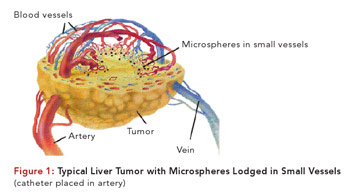
Toledo Radiological Associates (TRA) is pleased to announce a new treatment for unresectable liver cancers, both primary and metastatic. Radioembolization is a minimally invasive liver cancer therapy that consists of the catheter-directed infusion of millions of microparticles containing radioactive yttrium-90 (Y-90). The product (TheraSphere) is injected by TRA interventional radiologists into the hepatic artery through a catheter, which allows the treatment to be delivered directly to the tumor.
TheraSphere treatment can generally be administered on an outpatient basis and does not usually require an overnight hospital stay. TheraSpheres, 100% reimbursed by Medicare and many commercial health insurers, are used to treat patients with unresectable primary and metastatic liver cancers and can be used as a bridge to surgery, ablation or transplantation. It can also be used to treat liver cancer patients with portal vein thrombosis.
TheraSphere Patient Information Booklet
For more information about HCC click here.
back to page menu
Learn more about Interventional Radiology:
